This page explains miscarriage management at BPAS.

We understand that being told you are having a miscarriage can be confusing and you may experience a mixture of feelings
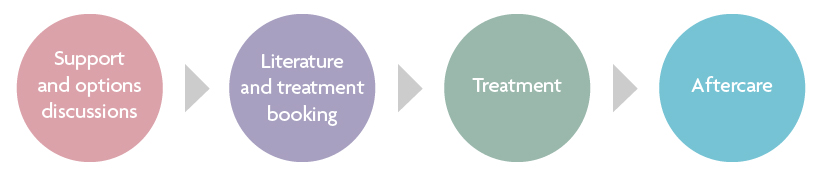
You may have been told by a healthcare provider other than BPAS that the pregnancy is no longer growing and that treatment may be necessary to remove it. Usually, your healthcare provider will offer treatment but if you are unhappy with the miscarriage treatment that has been proposed, we may be able to help. Call to enquire if we can treat you on behalf of the NHS.
Our staff will treat you sensitively and professionally, so if you have any questions, or would like anything explained further, please ask.

Treatment options
Your healthcare professional will discuss your treatment options with you, so don’t worry; we will explain all you need to know. Your treatment will depend on your symptoms, how many weeks the pregnancy is, medical suitability and your personal preferences.
If you've been diagnosed with a miscarriage at your treatment appointment, you may consider continuing with the treatment you have already planned.
BPAS offers surgical, medical and expectant miscarriage management. See below for a brief description with links to more information.

This is sometimes called ‘evacuation of retained products of conception’.
At less than 15 weeks of pregnancy you will be offered vacuum aspiration which involves removing the pregnancy through the cervix (neck of the womb) using gentle suction. This is usually carried out with local anaesthetic or moderate (conscious) sedation.
Dilatation and evacuation is the surgical method used from 15 weeks of pregnancy and involves instruments and suction to remove the pregnancy. This is normally carried out under moderate (conscious) sedation or general anaesthetic.
Advantages
- Surgical treatment usually completed in one visit
- If you are awake for the procedure, you know exactly what is going on.
- If you are anxious or worried about pain, you can be have some sedation for the procedure
Disadvantages
- Small chance of complications (all explained by our healthcare professionals)
- Must be done in the clinic
- May require treatment over 2 days if your pregnancy is in the second trimester

Involves using one or more medications to help you pass the pregnancy.
Please note, we are currently not offering medical miscarriage management in clinic. We continue to offer medical management at home for pregnancies under 10 weeks.
Usually, one medicine is given by mouth and the other is taken by placing tablets under your tongue or in your vagina. If you are less than 10 weeks pregnant you can take the medication with you to use at home.
Advantages:
- Can feel more natural than surgery for some women
- Quicker than waiting for nature to take its course
- Avoids surgery and or being put to sleep
- You are more in control of when and where you pass the pregnancy
- Simple to take either in the clinic or you can take the medication home if the pregnancy is less than 10 weeks.
Disadvantages:
- Bleeding, cramping and side effects
- The exact time the pregnancy will pass is uncertain
- May need surgical treatment if the process does not complete, but this happens much less than waiting for nature to take its course
- Spotting can continue until your next period.

This is an option at BPAS if the pregnancy is less than 13 weeks of gestation.
It involves letting nature take its course. You will go home with instructions on what to expect and when to contact us if there's a problem or the pregnancy has not passed on its own - if it hasn’t, we may then talk to you again about alternative solutions.
Advantages:
- Avoids surgery or being put to sleep
- Can take place in the privacy of your own surroundings.
Disadvantages:
- The exact time the pregnancy will pass is uncertain
- If the process does not complete on its own, medical or surgical treatment may be needed.
What you need to know
Your treatment and care are designed with your needs, medical safety, and personal preferences in mind. Our service is focused on you and is based on miscarriage guidelines produced by the Royal College of Obstetricians and Gynaecologists (RCOG) and National Institute for Health and Care Excellence (NICE).
We understand that there may be a variety of things you are thinking and feeling concerning this miscarriage, so we will be guided by you.
If there is anything you are unsure of, or you would like us to explain further, please ask a member of our team.
You can choose to receive your miscarriage care from BPAS or we can refer you into your local NHS service. A referral into the NHS will be necessary if you have a medical issue we are unable to manage safely.
We offer the following miscarriage care:
Early miscarriage is where the pregnancy stops growing in the first 13 weeks of pregnancy. Late miscarriage is where the baby dies between 14 and 24 weeks of pregnancy. The most common symptoms of a miscarriage are pain and bleeding. Some women only have gradual loss of pregnancy symptoms like breast tenderness or nausea.
A miscarriage is usually diagnosed by a combination of symptoms and one or more ultrasound scans. Sometimes blood tests are used.
It is not always possible to diagnose a miscarriage on the first scan and another one will be needed in a weeks’ time. If having a confirmed diagnosis of miscarriage is important to you, you have the option to delay your treatment for a week for another scan to confirm diagnosis.
Once a diagnosis is made you will have the time to talk about your thoughts and feelings and discuss treatment.
Approximately 20% of women who know they are pregnant are at risk of having miscarriage in the first 3 months of pregnancy. After 13 weeks the risk of miscarriage is 1-2%. Most miscarriages happen as a ‘one-off’ event and there is a good chance of having a successful pregnancy in the future, should you want one.
The risk of early miscarriage increases with a woman’s age. At the age of 30 the risk of miscarriage is 1 in 5 (20%). The risk rises to 1 in 2 (50%) when at age 42. Additional factors such as health problems like poorly-controlled diabetes, smoking or heavy drinking can contribute to a miscarriage, however, there is no scientific evidence to show that stress does. Sex during pregnancy is not harmful or associated with miscarriage.
A lot is still unknown about why early miscarriage happens. One common reason is chromosome problems. After 13 weeks of pregnancy, you may consider having additional tests to help understand why you miscarried. We will discuss the testing options with you and how you can access them.
If at this point you would like to further discuss how you feel about the miscarriage, please do let us know. We can arrange for appointments just for the purpose of talking through your thoughts and feelings.
If you choose medical management at home or expectant management, you can bring the tissue back to us to dispose of or dispose of it yourself. All tissue from the procedure will be disposed of in a sensitive way. It is collected and stored separately from other clinical waste, before being sent for incineration (burning). If you have any specific wishes about how you would like the tissue to be disposed of, such as burial or cremation, please discuss this with a member of staff before you have your procedure.
How we can help?
We are an independent healthcare charity which for more than 55 years, has been advocating and caring for women and couples who decide to end a pregnancy.